United States: In 1979, a burgeoning physician in Sydney, Australia, Colin Sullivan, devised a groundbreaking experiment to address nocturnal breathing disturbances. After a protracted wait for a suitable candidate, he encountered a construction worker so plagued by sleep deprivation that he would nod off precariously atop scaffolding during his shifts.
The laborer suffered from sleep apnea—his airway intermittently collapsed, disrupting his nocturnal respiration and repeatedly rousing him from slumber. Yet, he rebuffed Sullivan’s suggestion of surgical intervention, the prevailing treatment of the era, involving a tracheostomy to facilitate uninterrupted airflow.
Sullivan was thus compelled to trial an unorthodox invention: an apparatus he describes as “a hefty swimming pool tube attached to a blower.” This contrivance, when paired with a nasal mask, directed a gentle stream of pressurized air into the worker’s nostrils, maintaining the patency of his airway. For the first time in years, the man experienced unbroken, restorative sleep.
“It was a profoundly transformative outcome,” Sullivan recounted. At the time, however, he could not have foreseen the monumental demand for what would become the continuous positive airway pressure (CPAP) machine. Obesity, a principal precipitant of sleep apnea, was only beginning to emerge as a widespread issue. In the wake of today’s obesity pandemic, nearly a billion individuals globally grapple with this affliction.
Despite CPAP’s efficacy, Sullivan soon discovered its limitations. “Many individuals struggle with its usage,” he observed, underscoring the heterogeneity of sleep apnea. As advancements unfold, they aim to enhance CPAP adaptability while offering alternative solutions. Here are the forefront innovations, as per experts.
Sleep Apnea and CPAP: Opportunities and Obstacles
Although CPAP machines have revolutionized treatment for millions, myriad patients face hurdles in their adoption. With proper support and tailored strategies, some of these impediments can be surmounted.
“I’ve relied on CPAP for 16 years but never truly felt rejuvenated,” shared Emma Cooksey, an advocate with Project Sleep. Among her challenges, and common to others, was an ill-fitting mask. Provided the device sans comprehensive guidance, she encountered comfort obstacles unaided. “Navigating CPAP comfort remains a critical gap,” she emphasizes.
Dr. Kevin Motz, an otolaryngologist and sleep apnea researcher at Johns Hopkins, echoes this sentiment. “It’s not a universal remedy,” he remarked. Nasal masks are generally optimal, yet masks encompassing the mouth cater to those with impaired nasal respiration. Sifting through an overwhelming array of options often necessitates expert input from respiratory therapists or specialized medical suppliers, a resource frequently inaccessible.
Within mere years of initiation, approximately half of CPAP users diminish usage or abandon it altogether. Left unaddressed, sleep apnea exacerbates severe health conditions, including cardiovascular disease, cerebrovascular events, and metabolic disorders.
Technological platforms leveraging cloud-based insights and telehealth have emerged to bolster CPAP adherence. Companies such as Lofta and Better Night provide remote expertise to optimize mask compatibility. Additionally, accessories like padded mask liners, hose management systems, and chin straps enhance usability, promoting compliance.
Behavioral interventions further complement CPAP adaptation. Consulting cognitive-behavioral therapists can alleviate insomnia, claustrophobia, or CPAP-induced anxiety.
Diagnosing the Root Cause
Identifying the underlying pathology is paramount. Sleep apnea encompasses diverse etiologies, and precise diagnostics dictate tailored interventions.
Snoring often signals apnea. “Snoring warrants scrutiny,” advises Sullivan, now an emeritus medical professor at the University of Sydney.
Commercial sleep trackers embedded in wearables or beds offer preliminary detection, though their reliability warrants further study. Should such devices indicate apnea, follow-up with a physician or sleep specialist is critical. Comprehensive polysomnography remains the gold standard.
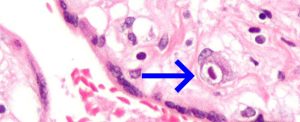
Sleep endoscopy, an invasive evaluation involving a micro-camera to localize airway obstructions, offers a roadmap for personalized therapy. Despite its utility, this procedure remains underutilized due to limited accessibility, Cooksey notes.
Pharmacological Frontiers
Two decades post-CPAP innovation, Dr. Atul Malhotra embarked on a quest to discover alternative therapies. His perseverance yielded fruit in the form of GLP-1 receptor agonists like tirzepatide. Preliminary findings indicate their efficacy in mitigating sleep apnea by addressing obesity-related airway obstruction. However, these pharmacological interventions are supplementary rather than curative, with sustained use and concomitant lifestyle modifications essential.
Lifestyle: A Cornerstone
Behavioral adjustments provide immediate benefits. Weight reduction, through balanced nutrition and physical activity, serves as a linchpin in ameliorating apnea severity.
“Even modest weight loss—a mere 10-15%—can halve the condition’s intensity,” notes Motz. Specific regimens, such as myofunctional therapy guided by speech pathologists, fortify airway musculature. Devices like eXciteOSA employ electrical stimulation to achieve similar outcomes.
Nutritional shifts towards plant-centric diets reduce systemic inflammation, a contributor to sleep apnea, according to Dr. Danny Eckert. However, the fatigue-induced hormonal cascade heightening hunger presents a formidable obstacle, as Cooksey attests.
Sleep hygiene—prioritizing consistent sleep schedules, exposure to natural daylight, and positional adjustments—further optimizes outcomes.
Surgical and Mechanical Alternatives
For recalcitrant cases, surgery offers an invasive recourse. Modern preoperative evaluations, including sleep endoscopy, enable targeted interventions. Techniques range from tissue restructuring to implanting devices like Inspire, which stimulates hypoglossal nerve activity to reposition the tongue, alleviating airway blockages.
Oral appliances designed to advance the lower jaw also hold promise. Custom-fitted by dentists trained in sleep medicine, these devices provide effective, albeit underutilized, solutions.
The Horizon Ahead
The quest for diversified, efficacious therapies continues. Innovations in pharmacology, neuromuscular devices, and surgical precision underscore a burgeoning era in sleep medicine.
“CPAP remains indispensable,” Sullivan reflected. “Yet, the horizon is replete with possibilities that promise to revolutionize treatment paradigms.”