A growing global crisis dubbed the “silent pandemic” is driven by multidrug-resistant bacteria, or superbugs, which defy traditional antibiotics.
A global conundrum, often termed a “silent pandemic,” has been stealthily engulfing the world. Unlike the dramatic flare-ups of viral outbreaks that capture headlines, this menace has expanded in a subdued yet persistent manner. What is the root cause of this crisis? Multidrug-resistant bacteria, colloquially dubbed superbugs.
The Rise of Superbugs: A Grave Threat
Superbugs exhibit formidable resistance to antibiotics, rendering traditional treatments ineffective. Over time, these bacteria adapt and evolve, acquiring the ability to withstand once-potent drugs. Alarmingly, they can also transmit their resistance traits to other microorganisms, compounding the severity of the situation, according to the reports by livescience.com.
In response, scientists are fervently pursuing innovative strategies to counteract this threat. From devising antibiotic alternatives to enhancing the efficacy of existing treatments, their efforts represent a crucial front in this escalating battle. Live Science has chronicled these advancements and the emergence of novel superbugs throughout 2024. Below are ten pivotal discoveries and narratives shaping our understanding of this crisis.
10 'superbug' stories from 2024, from bacterial 'Kryptonite' to deep-sea antibiotics #Science https://t.co/5xBEWmXCjd
— Pure Science 🔭🔬🧪🚀🧬🦖 (@Pur3Science) December 29, 2024
Vanquishing CRAB
A groundbreaking antibiotic has emerged to combat carbapenem-resistant Acinetobacter baumannii (CRAB), a notorious superbug resistant to most existing therapies. This novel drug belongs to a unique antibiotic class and disrupts the bacteria’s machinery for constructing outer membranes. Its highly selective action targets only A. baumannii, reducing the likelihood of fostering resistance in other bacterial species, as per the reports by livescience.com.
The Proliferation of “Hypervirulent” Strains
A particularly menacing strain, hypervirulent Klebsiella pneumoniae (hvKp), has surfaced across 16 nations, including the United States. Historically problematic in healthcare settings, classic K. pneumoniae strains predominantly afflicted immunocompromised individuals. However, hvKp defies this trend, causing aggressive infections even in individuals with robust immune defenses, as per livescience.com
Dormant but Dangerous: Persistent Superbugs
Recent research reveals that certain superbugs, including resistant strains of K. pneumoniae and E. coli, can persist within the human body for years—five and nine years, respectively. This prolonged residence heightens the risk of recurrent infections and increases the likelihood of transmitting these microbes to others. Moreover, these bacteria retain ample opportunities to exchange their resistance genes.
The Evolutionary Trade-offs of C. diff
The superbug Clostridioides difficile (C. diff), once known as Clostridium difficile, can rapidly develop resistance to primary treatment drugs. However, this adaptation incurs a cost, as resistant strains exhibit reduced growth efficiency. By understanding these evolutionary compromises, scientists aim to craft treatments that are more challenging for C. diff to outmaneuver, according to livescience.com.
Reverting Superbugs: A Bold Vision
Is it possible to dismantle a superbug’s defenses and render it vulnerable to antibiotics once more? Researchers are delving into revolutionary approaches to achieve this. One method involves utilizing bacteriophages—viruses that target bacteria—to reintroduce susceptibility genes into resistant strains. Other strategies focus on disrupting biofilm formation or inhibiting specific protein production, with the goal of extending the lifespan of current antibiotics.
Phage Therapy: A Resurrected Remedy
Amid the escalating resistance crisis, some scientists are revisiting phage therapy—a treatment predating antibiotics. Once overshadowed by the antibiotic revolution, phage therapy leverages viruses to combat bacterial infections. Science journalist Lina Zeldovich’s latest book spotlights pioneering efforts in this field, shedding light on its potential resurgence.
The Speed of Resistance Development
How swiftly can bacteria develop resistance? Evolutionary rates vary significantly among bacterial species, but resistance can emerge astonishingly fast—sometimes within days. Once a bacterium acquires resistance genes, it can disseminate them to neighboring cells, rapidly creating a resistant population, the reports by livescience.com mentioned.
Antibiotics from the Deep Sea
The quest for next-generation antibiotics has ventured into the ocean depths. Arctic Ocean microbes, particularly Actinobacteria, have been found to produce unique antibiotic compounds. Preliminary experiments indicate these compounds are effective against pathogenic E. coli, though clinical application remains a distant prospect.
Unveiling Heteroresistance
A peculiar resistance mechanism known as “heteroresistance” complicates treatment protocols. These microbes initially appear vulnerable to antibiotics but can abruptly activate resistance when exposed to certain doses. This phenomenon challenges traditional diagnostic methods and prolongs hospital stays, underscoring the need for better detection techniques, according to livescience.com.
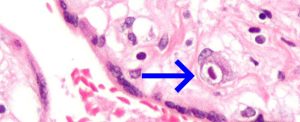
Emerging Fungal Threats: A New Contender
In China, researchers identified a previously unknown fungal infection caused by Rhodosporidiobolus fluvialis. Resistant to multiple first-line antifungal drugs, this fungus thrives in temperatures akin to the human body. As climate change accelerates, experts warn of the potential for similar pathogens to evolve heightened resistance, posing an additional layer of threat.